Locking Plate Series - Distal Tibial Compression Locking Bone Plate
Distal tibial Pilon fractures are rare, accounting for less than 10% of fractures around the ankle. The soft tissues at the distal tibia have poor tolerance to inadequate soft tissue coverage, which increases the difficulty of fracture treatment. Pilon fractures are known for comminution, displacement of the articular surface, and soft tissue injuries. Due to the changes in joint congruity and limb alignment, most fractures require surgical fixation. Definitive surgical treatment should be tailored to specific fracture types, soft tissue injuries, and patients. The appropriate timing of surgical treatment is the key to success.
Anatomical Features
Pilon fractures involve metaphyseal fragments, and sometimes diaphyseal fragments as well. There are also joint depression and comminuted fractures. There are always three basic bone fragments: the anterolateral fragment, the medial malleolar fragment, and the posterolateral fragment.
There are three typical areas of joint comminution: Lateral comminution occurs between the anterolateral and posterolateral fragments, usually close to the fibula. Central comminution may present as free bone fragments or compression of the posterolateral fragment. Medial comminution involves part of the medial fragment or compression adjacent to the medial malleolus.
Comminution usually occurs where the fracture lines intersect. Each of the three main fracture fragments may be comminuted and have additional fracture lines. It is important to protect the ankle blood vessels. The soft tissues should be handled carefully and only retracted when necessary to avoid wound - healing problems. Excessive stripping of the fracture fragments should be avoided to prevent avascular necrosis of the fragments.
Injury Mechanisms
High - energy injuries: Falls from a height, skiing, car accidents, etc. Low - energy injuries: Tripping on a flat surface.
Direction of violence: Axial compression; Rotational shear force; Varus shear force; Valgus shear force.
Varus force violence: More common in young people, with more severe trauma and high - energy injuries. The fracture line is in the sagittal plane, and the fibula is often intact.
Valgus force violence: More common in the elderly, with less severe trauma and low - energy injuries. The fracture line is in the coronal plane and is often associated with a fibular fracture.
Imaging Examinations
Routine standard anteroposterior, lateral, and mortise view X - rays of the ankle are taken. A full - length X - ray of the tibia can show the alignment and the knee joint above. For some patients with more complex fractures, X - rays of the contralateral limb are taken to provide a reference for fracture reconstruction and to detect pre - existing anatomical or congenital variations.
The injury mechanism can be predicted from the type of fibular fracture on X - rays and is classified as: Compressive violence (valgus deformity), Tensile violence (varus), Axial loading (intact fibula). If the fibula is intact, it is generally a severe partial intra - articular (Type B) injury. Axial loading injuries do not cause much displacement but result in a large amount of axial loading on the distal tibia, with multiple small articular surface fragments and a poor prognosis secondary to articular cartilage compression. The direction of fracture fragment displacement can be predicted from the lateral X - ray showing the type of talar displacement (usually anterior displacement).
Two - dimensional and three - dimensional CT reconstructions are essential. They can provide information including the degree of fracture comminution, the position and number of bone fragments, and the direction of displacement.
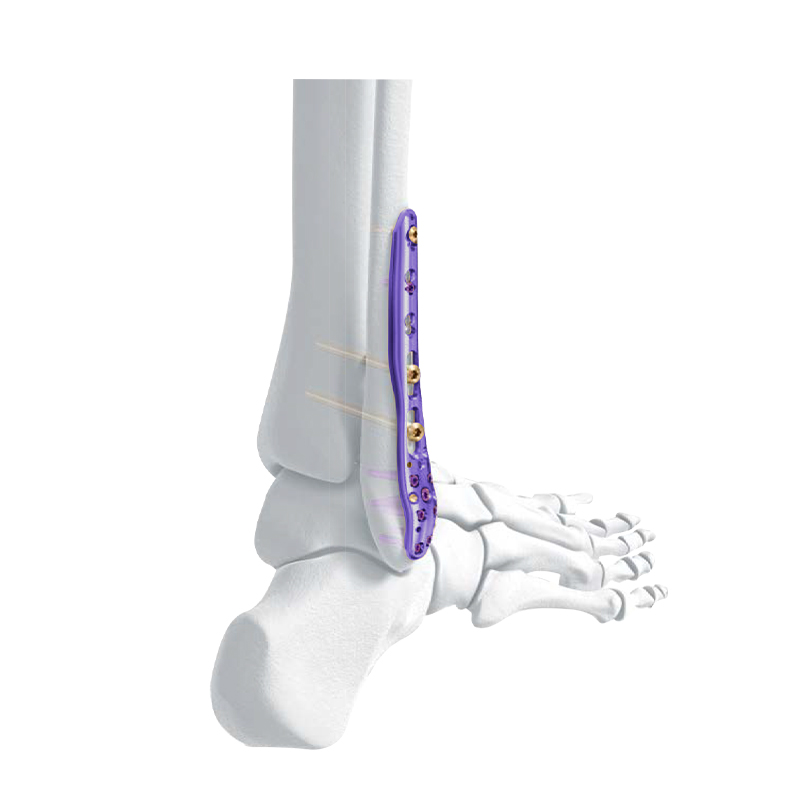
Distal Lateral Fibular Locking Plate
VA Distal Medial Tibia Locking Plate
Classification
AO/OTA Fracture - Dislocation Classification
Extra - articular Type A fractures usually appear simple but may be associated with significant soft tissue injuries. Typical partial intra - articular Type B fractures involve articular comminution and require buttress plates to reduce the intra - articular fragments. Complete intra - articular Type C fractures indicate high - energy injuries associated with comminution of the tibio - talar joint, injury to the distal tibio - fibular syndesmosis, fibular fractures, and tibial metaphyseal fractures, and are usually associated with severe soft tissue injuries.
Ruedi - Allgower Classification
Type I: A "T" - shaped split fracture without significant displacement.
Type II: Split of the articular surface with obvious displacement of the fracture line and moderate comminution.
Type III: Severe comminuted and compressive fractures of the distal tibial articular surface and metaphysis.
Non - surgical Treatment
Non - surgical treatment for distal tibial Pilon fractures is rare. The indications are minimally displaced fracture types and patients with comorbidities that increase the risk of surgical treatment. Extra - articular fractures with minimal changes in the overall tibial alignment can also be treated with plaster immobilization without surgery. A splint is initially used until the swelling subsides, and then a plaster cast is applied. Severe changes in the tibial or articular surface alignment may lead to problems with limb alignment and stability. Continuous X - ray examinations are necessary to ensure joint congruity and limb alignment.
Selective intra - articular fractures can also be treated non - surgically. For intra - articular fractures with less than 2 mm of fracture displacement and less than 3 mm of step - off, non - surgical treatment can be considered for patients with low functional requirements.
Surgical Indications
Articular surface step - off greater than 2 mm.
Valgus angulation greater than 5°.
Any varus angulation.
Open fractures.
Compartment syndrome.
Vascular injury.
Multiple injuries.
Surgical Timing
(1) Emergency treatment: Reduction and fixation of dislocations; Open fractures; Associated vascular injuries; Compartment syndrome.
(2) First - stage (Restoration of limb length and alignment): Calcaneal traction; External fixation; Reduction and internal fixation of fibular fractures, limited open reduction and internal fixation of posterior tibial malleolar fractures; Thrombus prevention.
(3) Second - stage: Approximately 10 - 14 days later, open reduction and internal fixation of the tibial fracture.
(4) The soft tissue conditions for the second - stage surgery are: Absorption of hematoma at the surgical site, epidermal regeneration at the fracture blisters, healing of the wound of open fractures without infection, subsidence of soft tissue edema, and wrinkling of the skin.
Surgical Approaches
(1) Maximize the exposure of the fracture line.
(2) Solve all fractures with the fewest surgical approaches.
(3) Avoid areas with poor soft tissue conditions.
(4) Consider the injury mechanism.
(5) Consider the plate placement position.
For fractures with varus deformity, a medial buttress plate is selected, and an anteromedial approach is used.
For fractures with valgus deformity, a lateral buttress plate is selected, and an anterolateral approach is used.
The distance between the two incisions should be at least 5 - 7 cm.
CZMEDITECH Products
English
Français
Русский
Español
العربية
Português
Deutsch
italiano
日本語
한국어
Nederlands
Tiếng Việt
ไทย
Polski
Türkçe
አማርኛ
ພາສາລາວ
ភាសាខ្មែរ
Bahasa Melayu
ဗမာစာ
தமிழ்
Filipino
Bahasa Indonesia
magyar
Română
Čeština
Монгол
қазақ
Српски
हिन्दी
فارسی
Kiswahili
Slovenčina
Slovenščina
Norsk
Svenska
українська
Ελληνικά
Suomi
Հայերեն
עברית
Latine
Dansk
اردو
Shqip
বাংলা
Hrvatski
Afrikaans
Gaeilge
Eesti keel
Māori
नेपाली
Oʻzbekcha
latviešu
অসমীয়া
Aymara
Azərbaycan dili
Bamanankan
Euskara
Беларуская мова
भोजपुरी
Bosanski
Български
Català
Cebuano
Corsu
ދިވެހި
डोग्रिड ने दी
Esperanto
Eʋegbe
Frysk
Galego
ქართული
guarani
ગુજરાતી
Kreyòl ayisyen
Hausa
ʻŌlelo Hawaiʻi
Hmoob
íslenska
Igbo
Ilocano
Basa Jawa
ಕನ್ನಡ
Kinyarwanda
गोंगेन हें नांव
Krio we dɛn kɔl Krio
Kurdî
Kurdî
Кыргызча
Lingala
Lietuvių
Oluganda
Lëtzebuergesch
Македонски
मैथिली
Malagasy
മലയാളം
Malti
मराठी
ꯃꯦꯇꯥꯏ (ꯃꯅꯤꯄꯨꯔꯤ) ꯴.
Mizo tawng
Chichewa
ଓଡ଼ିଆ
Afaan Oromoo
پښتو
ਪੰਜਾਬੀ
Runasimi
Gagana Samoa
संस्कृत
Gaelo Albannach
Sepeti
Sesotho
chiShona
سنڌي
Soomaali
Basa Sunda
Wikang Tagalog
Тоҷикӣ
Татарча
తెలుగు
ትግንያውያን
Xitsonga
Türkmençe
संस्कृत
ئۇيغۇرچە
Cymraeg
isiXhosa
ייִדיש
Yorùbá
isiZulu