Scaphoid Fracture
Scaphoid fracture is the most common carpal fracture, accounting for approximately 70% of all carpal bone fractures. Due to its unique anatomical position within the carpal bone arrangement, fresh scaphoid fractures are frequently missed in clinical diagnosis. Moreover, the peculiar vascular supply of the scaphoid predisposes patients to complications such as nonunion, avascular necrosis (AVN), and carpal instability in later stages. Clinically, scaphoid fractures are difficult to treat and often leave sequelae such as persistent wrist pain, restricted range of motion, and post-traumatic arthritis.
Unique Anatomical Role of the Scaphoid
The scaphoid is the longest bone in the proximal carpal row, shaped like a small boat (hence the name “scaphoid”). It spans between the proximal and distal carpal rows, playing a key role in stabilizing and connecting both rows. Normal wrist motions, including flexion, extension, radial deviation, and ulnar deviation, all depend on the coordinated movement of the scaphoid. Once fractured, the biomechanics of the entire wrist joint are disrupted.
Fragile Vascular Supply
The scaphoid receives blood supply mainly from branches of the radial artery, entering from the dorsal ridge and distal pole:
Approximately 70–80% of blood flow enters via the distal tubercle, flowing retrograde to nourish the proximal pole.
Only a few branches directly enter the proximal pole.
Implications: The closer the fracture is to the proximal pole, the greater the risk of vascular disruption.
Once blood flow is interrupted, the proximal fragment is highly prone to AVN and nonunion.
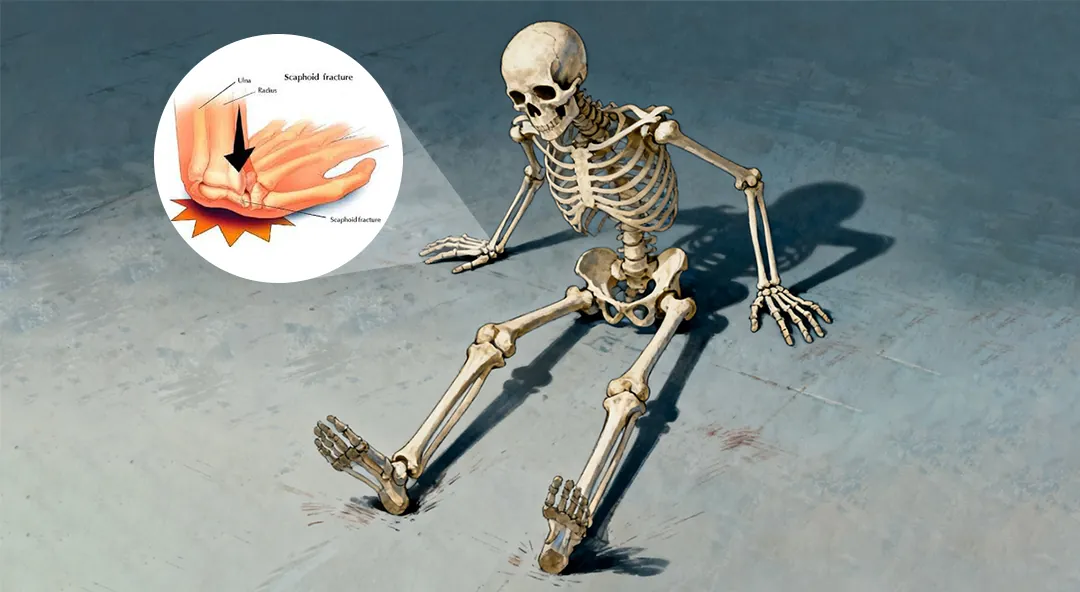
Common Injury Mechanism
The most common mechanism of injury is a fall onto an outstretched hand (FOOSH).When falling, individuals instinctively extend the arm and spread the fingers to absorb the impact with the palm. This frequent injury mechanism has drawn substantial clinical and research attention, and is widely referred to by the acronym FOOSH.
Delayed Diagnosis of Scaphoid Fracture
Scaphoid fractures often result from FOOSH injuries. In mild cases, symptoms may be limited to slight wrist pain, leading patients to neglect seeking medical care. Even when X-rays (AP and lateral views) are taken, fractures may not be immediately visible. Patients may return months later with progressive wrist pain, at which point imaging reveals a chronic scaphoid fracture—significantly delaying diagnosis and missing the optimal treatment window.
Key diagnostic recommendations:
X-ray imaging should be performed for all wrist injuries, including scaphoid views when fracture is suspected.
If X-rays are negative but suspicion remains, immobilization should be applied, followed by repeat imaging after 2 weeks.
Early immobilization can serve as both a diagnostic and therapeutic measure.
Treatment Options
External Fixation
Fresh, nondisplaced fractures can be treated with immobilization. However, fixation must be rigid to ensure healing. Standard plaster or resin splints may fail to control wrist and forearm rotation, reducing stability.
Plaster Cast Immobilization:
Long-arm thumb spica cast:
Indicated for proximal one-third fractures (highest AVN risk), vertical/oblique fracture lines, and initial diagnosis cases.
Immobilizes elbow at 90°, forearm, wrist, and thumb.
Provides maximum stability by eliminating forearm rotation.
Short-arm thumb spica cast:
Suitable for distal third fractures, tuberosity fractures, and stable mid-waist fractures (later stage).
Offers more comfort but less stability.
Internal Fixation
Headless Compression Screw (Herbert Screw)
Currently the gold standard for scaphoid waist fractures.
Herbert Cannulated Compression Screw
Bevelled Cannulated Herbert Screw
Kirschner Wire (K-wire) Fixation
A traditional yet useful method, often adjunctive.
Advantages: flexible, inexpensive, minimal disruption of vascularity.
Disadvantages: less stable, requires external fixation, infection risk, removal needed post-healing..
Indications: pediatric fractures, temporary fixation in comminution, adjunct to screw fixation.
Cannulated Screw Partially-threaded
Cannulated Screw Partially-threaded
Scaphoid Nonunion
Due to its unique vascular supply, scaphoid waist and proximal fractures are prone to nonunion and AVN.
Treatment: Bone grafting (non-vascularized or vascularized) combined with internal fixation (Herbert screw or K-wire). Precise graft placement and smooth articular surface restoration are crucial. In certain cases, radial styloidectomy may be required if bone prominence impinges during wrist motion.
Global Top 10 Herbert Screw Suppliers and CZMEDITECH Product Overview
The treatment of scaphoid fractures is of vital importance—not only for restoring wrist function but also for maintaining patients’ quality of life and work ability. Selecting the proper internal fixation device is key to preventing complications, achieving precise fixation, and promoting rehabilitation.
Among various implants, the Herbert Screw stands out due to its unique design and proven clinical performance, making it one of the most important devices in scaphoid fracture management.
Top 10 Herbert Screw Suppliers Worldwide
| Rank | Company Name | Logo |
| 1 | DePuy Synthes | ![Herbert Cannulated Compression Screw]() |
| 2 | Stryker | ![Herbert Cannulated Compression Screw]() |
| 3 | Zimmer Biomet | ![Herbert Cannulated Compression Screw]() |
| 4 | Arthrex | ![Herbert Cannulated Compression Screw]() |
| 5 | Smith & Nephew | ![Herbert Cannulated Compression Screw]() |
| 6 | Wright Medical Group | ![Herbert Cannulated Compression Screw]() |
| 7 | Acumed | ![Herbert Cannulated Compression Screw]() |
| 8 | aap Implantate AG | ![Herbert Cannulated Compression Screw]() |
| 9 | Orthofix | ![Herbert Cannulated Compression Screw]() |
| 10 | CZMEDITECH | ![Herbert Cannulated Compression Screw]() |
CZMEDITECH Herbert Screw Products
As a leading Chinese manufacturer and supplier of orthopedic implants, CZMEDITECH provides a comprehensive portfolio of Herbert Screws tailored for scaphoid fractures and other small bone injuries.
Key Features:
Headless compression design: ensures stable fixation while minimizing articular cartilage irritation.
High biomechanical stability: reliable interfragmentary compression promotes solid union.
Material options: available in medical-grade stainless steel and titanium alloy, with excellent biocompatibility and corrosion resistance.
Minimally invasive compatibility: suitable for both percutaneous and open approaches.
Multiple specifications: wide range of diameters and lengths to address diverse clinical needs.
Clinical Advantages:
Facilitates rapid and reliable scaphoid fracture healing, especially in high-risk waist and proximal pole fractures.
Enables early wrist mobilization, reducing stiffness and improving functional recovery.
Significantly lowers risk of nonunion and AVN compared to traditional fixation methods.
CZMEDITECH Products
English
Français
Русский
Español
العربية
Português
Deutsch
italiano
日本語
한국어
Nederlands
Tiếng Việt
ไทย
Polski
Türkçe
አማርኛ
ພາສາລາວ
ភាសាខ្មែរ
Bahasa Melayu
ဗမာစာ
தமிழ்
Filipino
Bahasa Indonesia
magyar
Română
Čeština
Монгол
қазақ
Српски
हिन्दी
فارسی
Kiswahili
Slovenčina
Slovenščina
Norsk
Svenska
українська
Ελληνικά
Suomi
Հայերեն
עברית
Latine
Dansk
اردو
Shqip
বাংলা
Hrvatski
Afrikaans
Gaeilge
Eesti keel
Māori
नेपाली
Oʻzbekcha
latviešu
অসমীয়া
Aymara
Azərbaycan dili
Bamanankan
Euskara
Беларуская мова
भोजपुरी
Bosanski
Български
Català
Cebuano
Corsu
ދިވެހި
डोग्रिड ने दी
Esperanto
Eʋegbe
Frysk
Galego
ქართული
guarani
ગુજરાતી
Kreyòl ayisyen
Hausa
ʻŌlelo Hawaiʻi
Hmoob
íslenska
Igbo
Ilocano
Basa Jawa
ಕನ್ನಡ
Kinyarwanda
गोंगेन हें नांव
Krio we dɛn kɔl Krio
Kurdî
Kurdî
Кыргызча
Lingala
Lietuvių
Oluganda
Lëtzebuergesch
Македонски
मैथिली
Malagasy
മലയാളം
Malti
मराठी
ꯃꯦꯇꯥꯏ (ꯃꯅꯤꯄꯨꯔꯤ) ꯴.
Mizo tawng
Chichewa
ଓଡ଼ିଆ
Afaan Oromoo
پښتو
ਪੰਜਾਬੀ
Runasimi
Gagana Samoa
संस्कृत
Gaelo Albannach
Sepeti
Sesotho
chiShona
سنڌي
Soomaali
Basa Sunda
Wikang Tagalog
Тоҷикӣ
Татарча
తెలుగు
ትግንያውያን
Xitsonga
Türkmençe
संस्कृत
ئۇيغۇرچە
Cymraeg
isiXhosa
ייִדיש
Yorùbá
isiZulu