![image (1) image (1)]() Anterior cervical discectomy with decompression and implant fusion (ACDF) is one of the most commonly used surgical methods for the treatment of spinal cord-type and nerve root-type cervical spondylosis, cervical spine trauma and other disorders, and it has the advantages of initial stabilisation, high fusion rate, restoration of normal anterior convexity, and the absence of external fixation, etc. The common postoperative complications such as difficulty in swallowing, degeneration of the adjacent segments, laryngeal reentrant nerve paralysis, cerebrospinal fluid leakage, haematoma, infection, and intervertebral implant subsidence etc. The overall incidence of postoperative complications is about 8%.
Anterior cervical discectomy with decompression and implant fusion (ACDF) is one of the most commonly used surgical methods for the treatment of spinal cord-type and nerve root-type cervical spondylosis, cervical spine trauma and other disorders, and it has the advantages of initial stabilisation, high fusion rate, restoration of normal anterior convexity, and the absence of external fixation, etc. The common postoperative complications such as difficulty in swallowing, degeneration of the adjacent segments, laryngeal reentrant nerve paralysis, cerebrospinal fluid leakage, haematoma, infection, and intervertebral implant subsidence etc. The overall incidence of postoperative complications is about 8%.
![按钮 按钮]()
In response to the above problems, the academic community is constantly working on technical improvements, conceptual breakthroughs, and prosthesis optimisation. The self-stabilising cervical spine fusion device (zero-trace), which is fully accommodated in the intervertebral space and effectively reduces the risk of postoperative dysphagia and adjacent segment degeneration, has been widely accepted.
The postoperative complications associated with prostheses are discussed below ——
1.Controversy over whether or not to resect the hooked vertebral joint
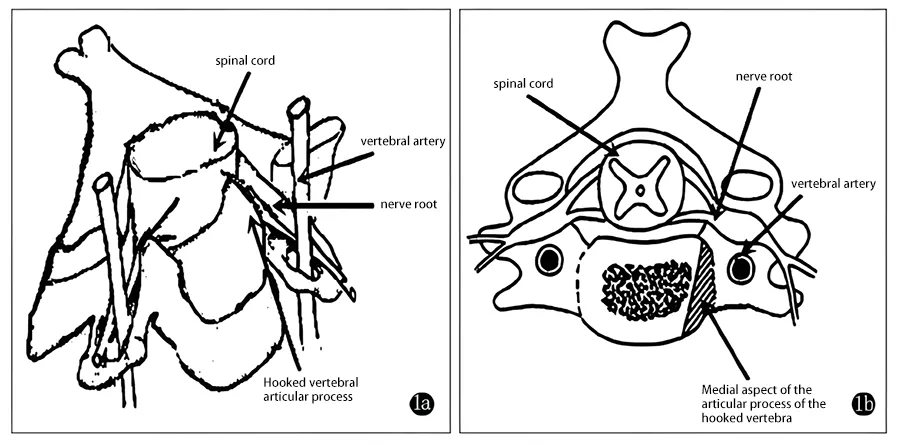
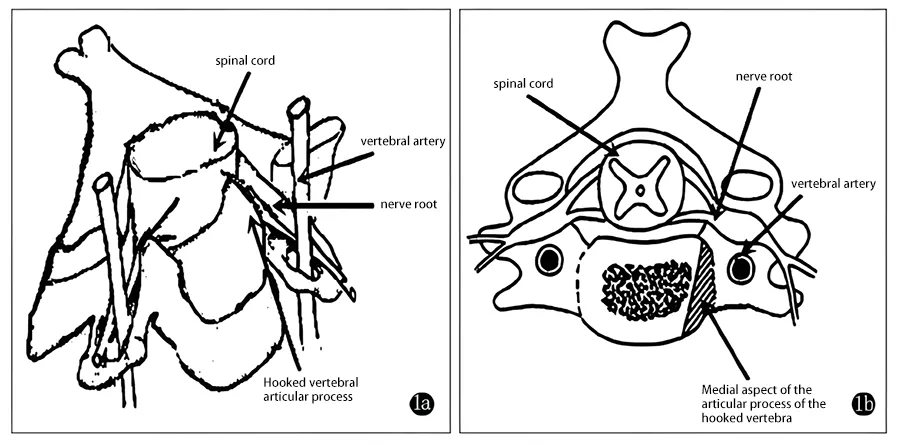
Fig. 1 Schematic diagram of the structure of the conotruncus, vertebral artery, and spinal cord and nerve roots.
a. Relationship between the articular eminence of the concha and the vertebral artery.
b. In the book, the medial edge of the articular eminence is removed, and the lateral edge is preserved appropriately to avoid damage to the vertebral artery.
![2_upscayl_2x_realesrgan-x4plus 2_upscayl_2x_realesrgan-x4plus]()
Fig. 2 Schematic diagram of nerve root compression and decompression by spreading out the hyperplastic conical joints.
a. Bone growths and spinal degeneration of the conical joints reduce the cross-sectional area of the intervertebral foramina, thus compressing the nerve roots.
b. Intervertebral fusion device/implant can open up the intervertebral space to enlarge the area of the intervertebral foramen and contact the nerve root compression, and at the same time, remodelling the stability of the spine.
The necessity of anterior cervical spine surgery to remove the hook vertebral joint has been a bone of contention since the inception of the technique
The first description of anterior cervical decompression and implant fusion with internal fixation was given by Robinson and Smith in 1955 in which he described the procedure as not requiring the removal of the leptokyphotic joint osteophyte. Cloward, another founder of the ACDF, emphasised that all compression should be removed, and that direct removal of the hyperplastic leptokyphosis was essential for decompression, while Robinson responded that the leptokyphosis could be resorbed as stability of the spine was established and as the abnormal mechanical forces disappeared, and that these instabilities were thought to be related to the formation of the leptokyphosis.
The preservationists argue that the hook joint contributes 48% to 60% of the stability of each segment and provides the greatest stability in the posterior aspect of the cervical spine, and that standard cervical foraminotomy decompression decompresses the posterior aspect of the hook joint and the anterior aspect of the neuraxial canal, whereas in reality the most stable part of the joint is removed, and instability as well as displacement of the implant position reduces the success of the fusion.
If equivalent clinical outcomes can be achieved without resection of the hook vertebral joint, preservation of the hook vertebral joint could theoretically provide the most appropriate setting for higher fusion rates. In addition, the preservation of the hook vertebral joint helps to reduce the chances of postoperative vertebral subluxation, and it has been noted that when the area of the hook vertebral joint is resected by more than 38%, the rate of interbody fusion subluxation will increase significantly.
![3_upscayl_2x_realesrgan-x4plus 3_upscayl_2x_realesrgan-x4plus]()
According to the resection school of thought, anatomically, the posterior wall of the leptospondylar joint is the anterior wall of the nerve root canal, and the bony residue from the leptospondylar joint hyperplasia can lead to intervertebral foraminal stenosis.
In current clinical practice, decompression by excision of the leptokyphosis is still advocated in patients with severe compression of the leptokyphotic joint hyperplasia, in order to relieve the compression of the nerve or vertebral artery as soon as possible.
Overall, controversy has always existed, but the choice of preserving, partially preserving, or completely removing the hook spondylolisthesis according to the patient's condition has become a consensus in various clinical practices. The individualised treatment strategy, however, places high demands on the size of the prosthesis.
![4_upscayl_2x_realesrgan-x4plus 4_upscayl_2x_realesrgan-x4plus]()
The common zero-cut traces on the market are limited by the need to screw in 4 screws for locking, and their width needs to be 17.5 mm, which is a large size for some nationals, and often requires partial occlusion of the hook joint for fusion implantation in the intervertebral space.
![9 9]()
The SAGI 2-nail locking zero incision has been reduced to 14.8 mm in width, taking into account the anatomical dimensions of the Chinese population, and provides the operator with a more personalised intraoperative treatment of the hook joint, allowing the treatment of the hook joint to be chosen according to the patient's actual condition, while ensuring initial stability and long-term fusion.
Postoperative spinal epidural haematoma
Spinal epidural haematoma (SEH) is a relatively rare and serious complication after anterior cervical approach, with an incidence of about 0.1% to 0.2%.SEH occurs in the rich venous plexus of the epidural, which will lead to severe spinal cord functional impairment if the haematoma formation is not treated in time. Emergency surgery after the diagnosis of SEH can help the recovery of neurological function.
![image (2) image (2)]()
Postoperative SEH schematic of ACCF
Spinal epidural haematomas are possible after both ACDF and ACCF, with ACCF having a higher risk of haematomas due to greater trauma and more oozing bone surfaces; however, the overall volume of the ACDF procedure is greater, with a higher number of SEHs occurring.
Prevention of SEH after anterior cervical approach should continue throughout the perioperative period:
A. Preoperative examination should be completed, and detailed enquiries should be made as to whether there are any coagulation diseases, and whether there is a history of long-term smoking and alcohol consumption; if there are people taking anticoagulant drugs, they should stop taking them for one week before the operation;
B. Thorough intraoperative haemostasis, incomplete haemostasis by electrocoagulation knife may lead to new bleeding, it is recommended to use bipolar electrocoagulation forceps; in the process of vertebral body subtotal resection, bone wax should be applied to avoid too much blood seepage from the bone surface; application of haemostatic drugs, such as tranexamic acid injection, etc., in order to reduce intraoperative bleeding; it is not necessary to seek for the complete resection of posterior longitudinal ligament of the operated segment, and the preservation of a small amount of posterior longitudinal ligament at the two sides can also achieve the effect of decompression; the placement of prosthesis should leave enough space at the right and left sides. When placing the prosthesis, enough space should be left on the left and right sides so that the epidural bleeding can flow to the front of the vertebrae and be discharged through the negative pressure drainage tube;
![10 10]()
C. After the operation, closely observe the vital signs; keep the drainage smooth; use anticoagulant drugs reasonably to avoid thrombosis; closely monitor the function of the nervous system; if there is any abnormality, deal with it in time.
![详情页8 详情页8]()
Designed to meet national anatomical dimensions
1. Provides a personalised clinical solution for the management of the hooked vertebral joint.
2. Reduce the chance of vertebral body subsidence
3. Reduce the risk of spinal epidural haematoma
Variable angle screw design for easy operation
![8 8]()
Screws with a coronal swing angle of -1.5°11.5° and a cephalad swing angle of 36°44° for easier intraoperative nail placement
No need to reserve extra space for screw insertion, the minimum incision is reduced from 2.5cm to about 2.0cm.
More adaptable to the concept of spinal endoscopic operation, realising Endo-ACDF.
![7 7]()
About CZMEDITECH
Cervical Peek Cage(2 or 4 Locking Screws) are precision orthopaedic solutions carefully developed by CZMEDITECH centred on anterior cervical discectomy decompression and implant fusion and driven by a global vision, dedicated to providing efficient, convenient and cost-effective comprehensive treatment solutions for patients with complex fractures around the world.
English
Français
Русский
Español
العربية
Português
Deutsch
italiano
日本語
한국어
Nederlands
Tiếng Việt
ไทย
Polski
Türkçe
አማርኛ
ພາສາລາວ
ភាសាខ្មែរ
Bahasa Melayu
ဗမာစာ
தமிழ்
Filipino
Bahasa Indonesia
magyar
Română
Čeština
Монгол
қазақ
Српски
हिन्दी
فارسی
Kiswahili
Slovenčina
Slovenščina
Norsk
Svenska
українська
Ελληνικά
Suomi
Հայերեն
עברית
Latine
Dansk
اردو
Shqip
বাংলা
Hrvatski
Afrikaans
Gaeilge
Eesti keel
Māori
नेपाली
Oʻzbekcha
latviešu
অসমীয়া
Aymara
Azərbaycan dili
Bamanankan
Euskara
Беларуская мова
भोजपुरी
Bosanski
Български
Català
Cebuano
Corsu
ދިވެހި
डोग्रिड ने दी
Esperanto
Eʋegbe
Frysk
Galego
ქართული
guarani
ગુજરાતી
Kreyòl ayisyen
Hausa
ʻŌlelo Hawaiʻi
Hmoob
íslenska
Igbo
Ilocano
Basa Jawa
ಕನ್ನಡ
Kinyarwanda
गोंगेन हें नांव
Krio we dɛn kɔl Krio
Kurdî
Kurdî
Кыргызча
Lingala
Lietuvių
Oluganda
Lëtzebuergesch
Македонски
मैथिली
Malagasy
മലയാളം
Malti
मराठी
ꯃꯦꯇꯥꯏ (ꯃꯅꯤꯄꯨꯔꯤ) ꯴.
Mizo tawng
Chichewa
ଓଡ଼ିଆ
Afaan Oromoo
پښتو
ਪੰਜਾਬੀ
Runasimi
Gagana Samoa
संस्कृत
Gaelo Albannach
Sepeti
Sesotho
chiShona
سنڌي
Soomaali
Basa Sunda
Wikang Tagalog
Тоҷикӣ
Татарча
తెలుగు
ትግንያውያን
Xitsonga
Türkmençe
संस्कृत
ئۇيغۇرچە
Cymraeg
isiXhosa
ייִדיש
Yorùbá
isiZulu








 Anterior cervical discectomy with decompression and implant fusion (ACDF) is one of the most commonly used surgical methods for the treatment of spinal cord-type and nerve root-type cervical spondylosis, cervical spine trauma and other disorders, and it has the advantages of initial stabilisation, high fusion rate, restoration of normal anterior convexity, and the absence of external fixation, etc. The common postoperative complications such as difficulty in swallowing, degeneration of the adjacent segments, laryngeal reentrant nerve paralysis, cerebrospinal fluid leakage, haematoma, infection, and intervertebral implant subsidence etc. The overall incidence of postoperative complications is about 8%.
Anterior cervical discectomy with decompression and implant fusion (ACDF) is one of the most commonly used surgical methods for the treatment of spinal cord-type and nerve root-type cervical spondylosis, cervical spine trauma and other disorders, and it has the advantages of initial stabilisation, high fusion rate, restoration of normal anterior convexity, and the absence of external fixation, etc. The common postoperative complications such as difficulty in swallowing, degeneration of the adjacent segments, laryngeal reentrant nerve paralysis, cerebrospinal fluid leakage, haematoma, infection, and intervertebral implant subsidence etc. The overall incidence of postoperative complications is about 8%.