The meniscus is a meniscus-shaped fibrocartilage with a triangular cross-section located between the tibial condyle and the plateau, which significantly improves femoro-tibial joint consistency and plays an important role in knee joint dynamics.
Normal And Abnormal Mri Findings
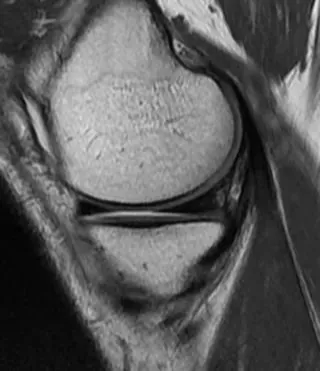
On sagittal and frontal images, the normal meniscus is triangular in hypointense. On the most lateral sagittal image, the meniscus is a "bow-tie" structure consisting of a mid-sagittal section combined with the anterior and posterior horns (Figure 1).
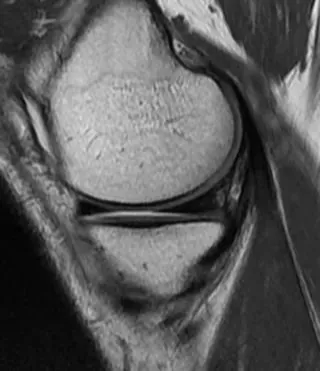
Figure 1 Normal MRI appearance of the medial meniscus. Proton density-weighted sagittal view: The anterior and posterior meniscal angles are homogeneous hypointense triangles. The meniscus is bow-shaped and consists of sections of the middle section that connect its anterior horns in front of it and its posterior horns behind it.
It is useful to understand certain anatomical abnormalities as they can simulate a meniscal split:
In sagittal section, the transition between the transverse and anterior ligaments;
popliteal tendon sheath;
Humphrey and Wrisberg's meniscus-femoral ligament connects the posterior horn of the lateral meniscus to the medial femoral condyle;
The oblique meniscus ligament, which occasionally connects the anterior horn of the meniscus to the posterior horn of the opposite meniscus, may mimic a migrating meniscus or barrel handle
Discoid meniscus is a rare congenital meniscus deformity. This meniscal dysplasia affects almost exclusively the lateral meniscus. Its "academic" diagnosis on MRI is based on seeing the continuity of the anterior and posterior horns on sagittal images in at least 3 consecutive 5 mm thick slices (Fig. 2). These findings are adjusted based on the partial settings used.
![discoid lateral meniscus]()
![discoid lateral meniscus1]()
Figure 2 Discoid lateral meniscus. Sagittal T1-weighted image. Continuity of front and rear corners on 3 consecutive 5mm fixed sections. Note the myxoid degeneration of the anterior horn of this discoid meniscus.
Meniscus Pathology Imaging
It is common practice to basically distinguish between traumatic meniscus and degenerative meniscus. Traumatic injuries result from the application of excessive mechanical force to a healthy meniscus. In young adults, the fissure is usually caused by indirect valgus injury, a sudden elevation of the tibia after external rotation or hyperflexion of the knee at 20° of flexion. Instead, degeneration occurs as a result of normal mechanical forces acting on the meniscus damaged by interstitial myxoid degeneration. Horizontal meniscal fissures may develop spontaneously or they may be caused by minor injuries.
Classification
According to the direction of the cleavage plane, fissures can be divided into horizontal fissures, vertical fissures or complex fissures
Horizontal Fissure
There is a split plane parallel to the tibial plateau that divides the meniscus into superior and inferior segments. These horizontal lesions are widespread, can significantly affect the medial or lateral meniscus, and are considered stable, although debris that migrates into the groove after damage to the medial meniscus has been described.
Vertical Fissure
Perpendicular to the tibial plane and along the circumference of the meniscus. These more commonly affect the medial meniscus. A complete injury is considered unstable and divides the meniscus into medial and lateral segments. The scanning level also includes the lateral meniscus body and the posterior horn of the meniscus, which is easy to be misdiagnosed as a barrel handle tear, which is more likely to occur when the knee joint is externally rotated. Combined with sagittal images, a barrel handle tear can be ruled out (Figure 3).
![Coronal MRI]()
A. Coronal MRI, the arrow points to the posterior horn of the lateral meniscus, which is easy to be misdiagnosed as barrel handle crack; B. When performing MRI scanning according to the position shown by the dotted line in the figure, a pseudo barrel handle tear will appear.
Radial fissures are perpendicular to the perimeter of the meniscus and usually affect the free edge of the meniscus.
Parrot Beak Tear
Is a mixed vertical damage consisting of a longitudinal component and a radial component cyclically extending at the free edge.
Finally, there are complex meniscal injuries, without any clear description, involving multiple horizontal and vertical fissures.
Mri Manifestations Of Meniscus Injury
Meniscus Tear
Stoller et al. suggested 3 grades of meniscus (Figure 4)
Grade 1: Hyperintensity nodular meniscus retained on the meniscus surface;
Grade 2: High signal linear meniscus retained on the meniscus surface;
Grade 3: Hyperintensity extends to one articular surface of the meniscus.
![meniscus]()
![meniscus1]()
![meniscus2]()
Figure 4 Stoller scale. a: Grade 1: One or more intermediate nodular hyperintensity sites associated with the articular surface of the meniscus; b: Grade 2: Linear intermediate hyperintensity on the articular surface of the meniscus; c: Grade 3: Linear intermediate hyperintensity extending to An articular surface of the meniscus.
Although the distinction between grades 2 and 3 is modest, it distinguishes degenerative intrameniscal hyperintensity (Figure 5) from true fissures. This distinction between a degenerated and torn meniscus is not always straightforward, and there are many sources of error due to the appearance of extra or missing.
![Degenerative appearance of the meniscus]()
Figure 5. The degenerative appearance of the meniscus. Sagittal proton density view with fat saturation. High signal areas can be seen without any true fracture linear image.
Precautions:
MRI has excellent performance, with sensitivity and specificity between 90% and 95%. On MRI, a meniscal cleft appears as an intermediate linear hypointense extension to one of the articular surfaces of the meniscus (Stoller grade 3), or a pure morphological abnormality.
When the tear is only visible on a single slice, there are some difficulties, especially the high risk of false positive results. If hyperintensity within the linear meniscus significantly affects the meniscal surface, i.e. in at least two adjacent sections, it is recommended to be considered pathological. This concept should be adapted depending on the image acquisition technique used (3 to 4 mm sections or obtaining a 3D volume with isotropic mm sections).
Radial meniscal clefts are sometimes more difficult to diagnose, given their orientation. These mainly lead to morphological abnormalities:
![Discontinuous or truncated appearance of the meniscus bowtie on the sagittal image]()
Figure 6. Radial fissure in the anterior segment of the medial meniscus in sagittal proton density-weighted view. Normal appearance of the medial meniscus truncated bow tie (arrow).
Rupture of the meniscus with a bucket handle complicates approximately 10% of longitudinally extending spondylolisthesis. In this case, the sensitivity of MRI is about 70%, depending on the diagnostic criteria used.
MRI findings that need attention:
The most common finding is the direct visualization of migrating fragments in the intercondylar region: the "double posterior cruciate ligament (PCL)" landmark is characteristic when the medial meniscus is damaged and the anterior cruciate ligament is intact. The dislocated segment appears as an arcuate hypointense band parallel to the normal posterior cruciate ligament, producing a "double PCL" appearance (Fig. 7). Excessive rake horns (over 6 mm in size) may also reflect the presence of a barrel handle (Figure 8). In this case, the dislocated meniscus fragment is attached to the healthy anterior horn.
![medial meniscus handle]()
Figure 7 The appearance of the medial meniscus handle has a "double PCL" sign. Sagittal PD-weighted view with fat suppression: The dislocated meniscus fragment (arrow) lies beneath the normal PCL (arrow) and forms the characteristic "double PCL" appearance.
![Half-moon itamae giant angle]()
Figure 8 Appearance of the front giant horn. Sagittal proton density weighted view. The anterior part of the dislocated fragment (arrow) is attached to the anterior meniscus angle (arrow). Note that the rear corners are not shown (*).
Other MRI findings:
Other MRI signs have been validated, such as missing bow tie, inverted meniscus sign, or meniscal fragments displaced directly into the intercondylar region on millimeter frontal images (Fig. 9) or axial images.
![Meniscus Fragment]()
Figure 9 Dislocated bucket handle in slot. Frontal PD-weighted view after fat suppression. The dislocated meniscus fragment (arrow) is in contact with the ACL (arrow).
Another formal sign of meniscal instability is the identification of peripheral displacement of meniscal fragments into the femoral meniscal recess or the femoral-tibial recess. These displacements involve almost exclusively the medical meniscus and are a complication of some horizontal cleft cases in 10% of cases. Coronal and transverse sections are the best way to identify these fragments.
Meniscus Detachment
Meniscal detachment occurs as a result of severe valgus injury and is caused by rupture of the meniscus' capsular appendage. These tend to affect the posterior horn of the medial meniscus that attaches to the joint capsule through a thickening of the joint capsule (the posterior oblique ligament).
They result in a 5 mm offset to the superior meniscus from the posterior border of the tibial plate on sagittal images (Fig. 11), or fluid insertion between the base of the meniscus and the plane of the joint capsule.
![Detachment of the posterior horn of the meniscus]()
Figure 11 Detachment of the posterior horn of the meniscus. Sagittal proton density view. The separated meniscus is displaced anteriorly. There is a large area of hyperintensity (*) between the base of the meniscus and the posterior capsule (arrow).
Floating Meniscus
This is the result of a violent injury and is due to meniscal-tibial ligament rupture and detachment of the medial portion of the meniscus. On MRI, the separated meniscus is completely surrounded by fluid and appears to "float" on the tibial plateau (Figure 12).
![floating meniscus]()
Figure 12 Floating meniscus. Frontal proton density view with fat saturation. The separated meniscus is surrounded by fluid, especially between its inferior surface and the tibial plateau (arrow).
Postoperative Meniscus
Recurrent pain after meniscectomy presents many diagnostic difficulties: recurrent fissures, postmeniscectomy, chondrolysis, subchondral necrosis, or arthralgia. MRI often fails to detect recurrent fissures because meniscectomy leaves intermediate hyperintensities that "wrongly" communicate with the meniscus surface. The only finding that was considered pathological and interpreted as a recurrent fissure was fluid intrameniscal hyperintensity on T2-weighted images. These limitations of simple MRI alone have prompted some authors to propose the use of MRI arthroscopy, although again the results here are inconsistent.
How to Buy Orthopaedic Implants and Orthopaedic Instruments?
For CZMEDITECH, we have a very complete product line of orthopedic surgery implants and corresponding instruments, the products including spine implants, intramedullary nails, trauma plate, locking plate, cranial-maxillofacial, prosthesis, power tools, external fixators, arthroscopy, veterinary care and their supporting instrument sets.
In addition, we are committed to continuously developing new products and expanding product lines, so as to meet the surgical needs of more doctors and patients, and also make our company more competitive in the whole global orthopedic implants and instruments industry.
We export worldwide, so you can contact us at email address song@orthopedic-china.com for a free quote, or send a message on WhatsApp for a quick response +86-18112515727.
If want to know more information,click CZMEDITECH to find more details.
English
Français
Русский
Español
العربية
Português
Deutsch
italiano
日本語
한국어
Nederlands
Tiếng Việt
ไทย
Polski
Türkçe
አማርኛ
ພາສາລາວ
ភាសាខ្មែរ
Bahasa Melayu
ဗမာစာ
தமிழ்
Filipino
Bahasa Indonesia
magyar
Română
Čeština
Монгол
қазақ
Српски
हिन्दी
فارسی
Kiswahili
Slovenčina
Slovenščina
Norsk
Svenska
українська
Ελληνικά
Suomi
Հայերեն
עברית
Latine
Dansk
اردو
Shqip
বাংলা
Hrvatski
Afrikaans
Gaeilge
Eesti keel
Māori
नेपाली
Oʻzbekcha
latviešu
অসমীয়া
Aymara
Azərbaycan dili
Bamanankan
Euskara
Беларуская мова
भोजपुरी
Bosanski
Български
Català
Cebuano
Corsu
ދިވެހި
डोग्रिड ने दी
Esperanto
Eʋegbe
Frysk
Galego
ქართული
guarani
ગુજરાતી
Kreyòl ayisyen
Hausa
ʻŌlelo Hawaiʻi
Hmoob
íslenska
Igbo
Ilocano
Basa Jawa
ಕನ್ನಡ
Kinyarwanda
गोंगेन हें नांव
Krio we dɛn kɔl Krio
Kurdî
Kurdî
Кыргызча
Lingala
Lietuvių
Oluganda
Lëtzebuergesch
Македонски
मैथिली
Malagasy
മലയാളം
Malti
मराठी
ꯃꯦꯇꯥꯏ (ꯃꯅꯤꯄꯨꯔꯤ) ꯴.
Mizo tawng
Chichewa
ଓଡ଼ିଆ
Afaan Oromoo
پښتو
ਪੰਜਾਬੀ
Runasimi
Gagana Samoa
संस्कृत
Gaelo Albannach
Sepeti
Sesotho
chiShona
سنڌي
Soomaali
Basa Sunda
Wikang Tagalog
Тоҷикӣ
Татарча
తెలుగు
ትግንያውያን
Xitsonga
Türkmençe
संस्कृत
ئۇيغۇرچە
Cymraeg
isiXhosa
ייִדיש
Yorùbá
isiZulu